
A spitting cobra can ship venom both via a chunk or by ejecting it from its fangs.Credit score: BlackBoxGuild/Creatas/Getty
Venomous snakes chunk hundreds of thousands of individuals yearly, most of them in India. Ravikar Ralph, a doctor on the Christian Medical Faculty Vellore hospital in India, is without doubt one of the individuals who treats them.
The hospital, certainly one of simply 9 poison-control centres in India, sees about 200 people who find themselves gravely sick after a snakebite annually. They arrive with a wide range of signs. Bites from venomous snakes known as vipers could cause bleeding and tissue injury that’s extreme sufficient to require amputation. The venom of kraits (Bungarus spp.) induces belly ache and progressive paralysis. Certainly one of Ralph’s sufferers, a farmer, spent 71 days in hospital after being bitten by an Indian cobra (Naja naja). He needed to endure dialysis as a result of his kidneys started to fail. A subsequent coronary heart assault required him to be resuscitated. “The chunk almost took his life,” Ralph says. The farmer was fortunate. Yearly, round an estimated 63,000 folks die from snakebites worldwide (see ‘Snakebite mortality’).
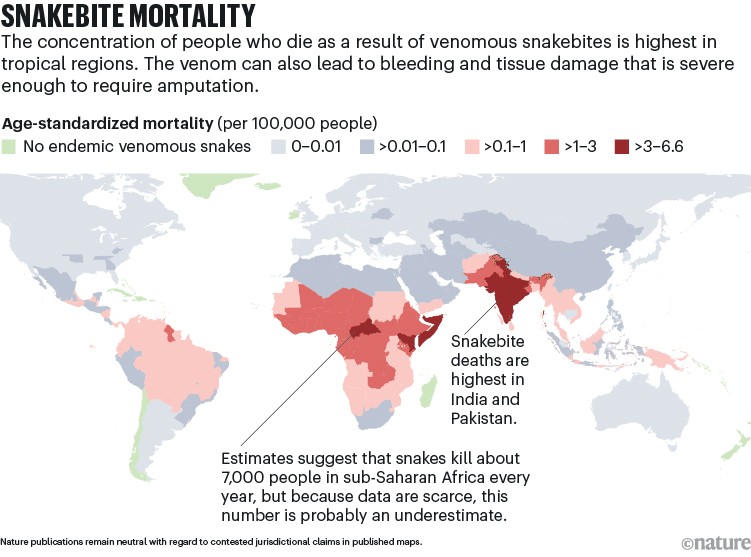
Supply: GBD 2019 Snakebite Envenomation Collaborators. Nature Commun. 13, 6160 (2022). Map credit score: Alisdair Macdonald
Antivenom is the one accepted remedy for snakebites. It’s produced in a lot the identical method because it was 100 years in the past. Small, non-lethal quantities of snake venom are injected into animals corresponding to horses, which then produce antibodies which might be collected from the animals’ blood. Antivenom saves lives, particularly when it’s administered quickly after the chunk.
However this therapy is difficult to return by within the rural areas the place most bites happen. And it has quite a lot of critical drawbacks. To maximise effectiveness, it’s nearly all the time given intravenously. And most often, antivenom solely works in opposition to the particular snake venom that was used to provide it. A horse injected with venom from a black mamba (Dendroaspis polylepis), for instance, gained’t produce antibodies that work in opposition to cobra venom. In response to one research1, there are 127 antivenoms available on the market.
A part of Nature Outlook: Uncared for tropical illnesses
What’s extra, as a result of antivenom comes from animals, it generally causes extreme immune reactions. “All of these deficiencies imply that there’s a extremely robust rationale to attempt to enhance therapy and to develop new therapies that may tackle a few of these challenges,” says Nicholas Casewell, a venom biologist on the Liverpool Faculty of Tropical Medication, UK.
A really perfect remedy to counteract venomous snakebites could be simple to manage and work in opposition to a variety of species. Researchers have made important headway in direction of these targets previously a number of years. They’re testing repurposed medicines in medical trials, discovering drug targets in snake venom and creating antibodies that appear to counteract venom, not less than in animal fashions. Ultimately, they goal to mix these next-generation therapies into cocktails that might be efficient in opposition to venoms from many species of snake. However for these therapies to achieve the individuals who want them most, additionally they need to be reasonably priced.
Well timed therapy
Snakebites are so lethal, partly, as a result of the people who find themselves bitten usually reside removed from the closest provide of antivenom. Due to the necessity for intravenous supply and the chance of extreme uncomfortable side effects, it’s sometimes out there solely in hospitals. Sadly, many people who find themselves bitten by no means make it there. Or, in the event that they do, by the point they arrive the injury is so widespread that antivenom doesn’t present a lot profit. That’s why researchers have lengthy hoped to seek out medicines that may be given quickly after the chunk happens, even earlier than the particular person arrives at a hospital.
The duty is trickier than it sounds. Snake venoms are complicated concoctions that encompass dozens of poisons. Precisely what they comprise varies not simply between species, but additionally throughout the similar species. The excellent news is that solely a handful of toxin households in snake venom are lethal to people. Researchers have already recognized medicines that appear to focus on three of those. As a result of these are present medicines — drugs or injectables — they don’t have to begin the drug-development course of from scratch. And that ought to hold prices down.
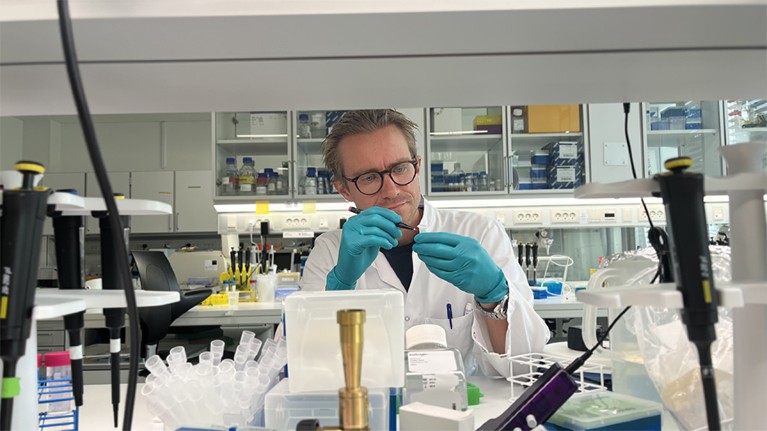
Antibody researcher Andreas Laustsen-Kiel marks samples in his laboratory on the Technical College of Denmark in Kongens Lyngby.Credit score: Emily Urvi Glegg-Sørensen
Matthew Lewin, an emergency-medicine doctor and neuroscientist primarily based in California, started creating therapies for snakebite greater than a decade in the past. He was placing collectively discipline kits for a California Academy of Sciences’ expedition to the Philippines and lamenting the truth that he didn’t have a lot to supply. Antivenom is troublesome to manage within the discipline.
Lewin thought he may be capable of discover an present remedy that might function a remedy, ideally one thing that wouldn’t should be injected, corresponding to a tablet. “You’ll be able to take them orally, they get out into the circulation quick, they will penetrate tissues that the antivenom can’t,” he says. However he didn’t make a lot progress on the mission till an opportunity encounter at a home celebration in California. Former Speaking Heads guitarist and expertise investor Jerry Harrison occurred to be there, and he requested “Does anyone have any loopy concepts which might be mendacity fallow?” Lewin jumped on the likelihood to share his imaginative and prescient for a snakebite remedy. Harrison was intrigued.
In 2015, the pair co-founded biotechnology agency Ophirex in Corte Madera, California. The corporate is specializing in an anti-inflammatory drug, known as varespladib, that had been examined in additional than 2,500 folks with coronary heart issues. It was by no means accepted as a result of it didn’t appear to assist the center. However in experiments that started in Lewin’s storage, he found that varespladib does appear to inhibit a household of enzymes known as secretory phospholipases A2 (sPLA2), toxins which might be discovered within the venom of 95% of venomous snakes. “That’s actually the venom element that’s prone to kill you,” he says.
In 2021, Ophirex began human trials on the drug to deal with snakebite. The corporate’s first research enrolled 95 people in India and the USA who had been bitten by any venomous snake throughout the earlier ten hours2. All of those people obtained the usual of care, together with antivenom. Round half obtained varespladib, and the rest obtained a placebo. People who obtained the drug didn’t fare any higher than those that didn’t. Each teams skilled about the identical quantity of enchancment within the hours after initiating the research. However Lewin says that there are hints that varespladib does what it’s meant to do if given quickly after the chunk. When the researchers checked out people who had been enrolled within the research inside 5 hours of being bitten, they discovered that the varespladib group fared barely higher by some measures, though the variations weren’t statistically important. That means that the tablet, if given rapidly, may purchase folks extra time to achieve the hospital, providing them what Lewin calls “a bridge to survival”.
Lewin hopes {that a} second research that may wrap up quickly will present a extra definitive reply as to whether varespladib works as meant to inhibit the consequences of venom sPLA2s. On this trial, researchers are administering the drug intravenously in order that it enters the bloodstream rapidly. Giving a drug on this method isn’t sensible within the discipline, however Lewin hopes that it would assist to show the drug’s efficacy.
Casewell and his colleagues are hoping to repurpose a unique oral remedy to deal with snakebites. Unithiol is used to deal with heavy-metal poisoning. It binds to steel ions and neutralizes them till they are often excreted in urine. In individuals who have been bitten by a snake, unithiol disables metalloproteinase enzymes, that are among the many commonest and lethal teams of poisons discovered within the venom of many vipers. These enzymes trigger a bunch of issues, together with bleeding. Unithiol works by mopping up the zinc ions that this group of enzymes must perform.
Experiments in animals have been encouraging. The gold-standard check for antivenom therapies includes mixing the remedy with a deadly dose of snake venom and delivering it intravenously to mice. In that situation, unithiol labored. However more and more, researchers are utilizing ‘rescue’ fashions that extra intently mimic what occurs in actual life. The venom is run first, adopted by the remedy. Casewell and his colleagues injected mice with a deadly dose of venom from a West African saw-scaled viper (Echis ocellatus) after which gave the mice unithiol, antivenom or each. Unithiol carried out about in addition to antivenom, and all of the mice that obtained unithiol quarter-hour after an injection of the venom, after which standard antivenom after one hour, survived for twenty-four hours — the top of the experiment3.
Casewell’s group has already moved unithiol into security trials in people. It examined various doses of the therapy in adults in Kenya who had been wholesome and who had not been bitten by a snake4. Casewell has secured funding for an efficacy trial, which he hopes to begin quickly.

Antibody researcher Andreas Laustsen-Kiel (left) talks to a employees member on the Nairobi Snake Park who’s holding a species of African cobra.Credit score: Andreas Laustsen-Kiel
Additional work by Casewell and his colleagues suggests a typical blood thinner can act in opposition to a 3rd household of poisons, often called three-finger toxins5. The researchers used CRISPR gene-editing expertise to develop a pool of human cells that had a wide range of single genes inactivated. They then uncovered these cells to venom from two species of spitting cobra (a chunk from these snakes could cause large tissue dying). The display screen helped the researchers to know which parts of the cells are required for the venom to trigger cell dying. Manufacturing of sugar molecules appears to be key. Cells that lacked these genes had been proof against the venom’s poisonous results. The researchers puzzled whether or not they might use a molecule formed like these sugars, such because the frequent blood thinner heparin, to bind to the toxins and forestall them from inflicting injury. It labored. In mice, a heparin-like drug known as tinzaparin curbed native tissue injury after the rodents had been injected with spitting cobra venom.
“This particular kind of toxin can do some actually nasty injury to your tissue,” says Steven Corridor, one of many co-authors and a pharmacology researcher at Lancaster College, UK. “So having one thing that may goal these toxins is probably very highly effective.”
Casewell agrees that these blood thinners are “available, they’re cheap, they’ve been licensed for a very long time, they usually have very well-defined security profiles”, he says. And since they’re secure and may be injected underneath the pores and skin, they may very well be used within the communities through which folks get bitten, maybe with the assistance of a pharmacist. The hope is that they’d stave off tissue injury, giving a person extra time to achieve hospital.
Every of those medication might show useful, and the subsequent step is to get them accepted individually for snakebites. However most researchers anticipate that the perfect drug therapies might be cocktails that concentrate on a number of toxins. Final yr, Corridor, Casewell and their colleagues reported that injecting varespladib with both unithiol or marimistat, one other drug that targets metalloproteinases, drastically lowered tissue dying brought on by viper venom in mice6. The mix labored even when delivered an hour after the venom was injected. “We had been identical to, ‘Holy crap, that is improbable!’” Corridor says. The group examined venoms from vipers in Central America, the USA and West Africa. The mix labored in opposition to all of them.
Corridor is already fascinated with attainable combos. “We now have [drug candidates] that may goal not less than these three totally different main toxin households,” he says. “You’d have a tough time discovering any snake venom that doesn’t comprise not less than a kind of households as a significant element.”
Antibody antidote
Though small molecules corresponding to varespladib might show useful, they aren’t prone to exchange antivenom. So, many researchers are working to overtake a remedy they already know is efficient: antibodies.
“Present antivenoms are primarily based on antibodies,” says Andreas Laustsen-Kiel, an antibody researcher on the Technical College of Denmark in Kongens Lyngby. “They work. They neutralize venom toxins.” However every product sometimes works solely on a handful of species. Researchers hope to seek out extra common antibodies that act in opposition to a spread of snake venoms after which produce them within the lab. Like standard antivenom, lab-made antibodies are administered intravenously. However the hope is that they’d be easier to provide and fewer prone to trigger an allergic response.
Joseph Jardine, an immunologist at Scripps Analysis in La Jolla, California, has spent a lot of his profession engaged on HIV. He first stumbled into creating snakebite therapies in 2020. On the time, he was working for a non-profit group that develops vaccines for infectious illnesses. He knew little about snakes. However the fundamental drawback appeared acquainted: how do you develop antibodies that may neutralize a goal that has an infinite quantity of variability? “That is nearly precisely the identical state of affairs as HIV,” he says. In each circumstances, the answer is to develop antibodies that bind to the components which might be conserved — the buildings of the goal which might be so essential they will’t change.
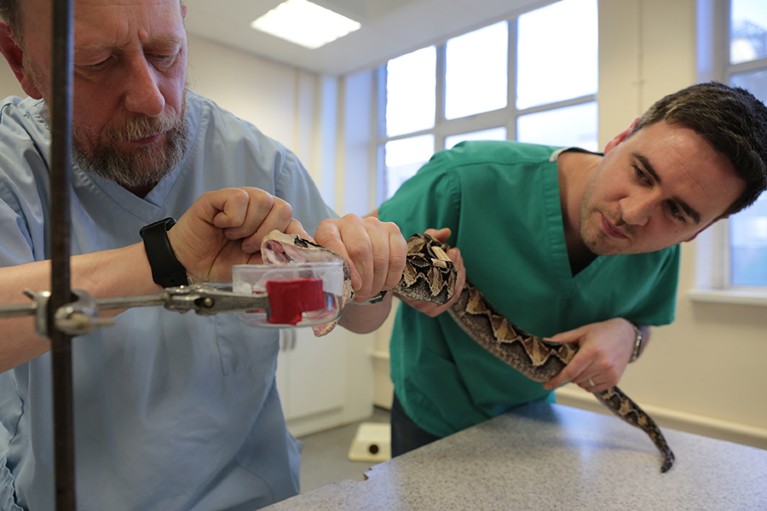
Venom biologist Nick Casewell (proper) helps to extracts venom from a Gaboon viper (Bitis gabonica).Credit score: Kirstin Kidd
Jardine and his colleagues are focusing first on three-finger toxins. They created an artificial model after which searched a library of fifty billion human antibodies to search for something that may bind to it. They discovered a number of thousand promising candidates and additional winnowed their listing all the way down to 30 by testing them in opposition to three-finger toxins from 4 species of snake. One clear winner stood out: an antibody known as 95Mat5. This antibody, administered 10 or 20 minutes after mice had been dosed with venom from a black mamba or monocled cobra (Naja kaouthia), rescued the rodents from the neurotoxic results of the three-finger toxins. The entire mice handled with 95Mat5 survived for twenty-four hours, the top of the statement interval. Mice that didn’t obtain the antibody died inside three hours7.
Now, Jardine and his colleagues are trying to find antibodies that work as properly in opposition to the opposite households of poisons. “The dream that we’ve is to have the ability to exchange the present antivenoms with 4 or 5 actually good, broadly neutralizing monoclonal antibodies,” he says.
Lab-made human antibodies aren’t low cost to provide, nonetheless. So Laustsen-Kiel and his colleagues have began pursuing a unique sort of remedy. Moderately than creating human antibodies, they’re creating nanobodies: a a lot smaller kind of antibody produced by animals corresponding to llamas and alpacas (see ‘The nanobody various’). Nanobodies are much less complicated than antibodies, to allow them to be produced within the lab utilizing organisms corresponding to yeast or Escherichia coli, making them considerably inexpensive. “You’ll be able to possible go an order of magnitude down in value of producing,” Laustsen-Kiel says. They usually’re “tremendous steady”, he provides. “You’ll be able to warmth them up, nearly boil them, they usually keep intact.”
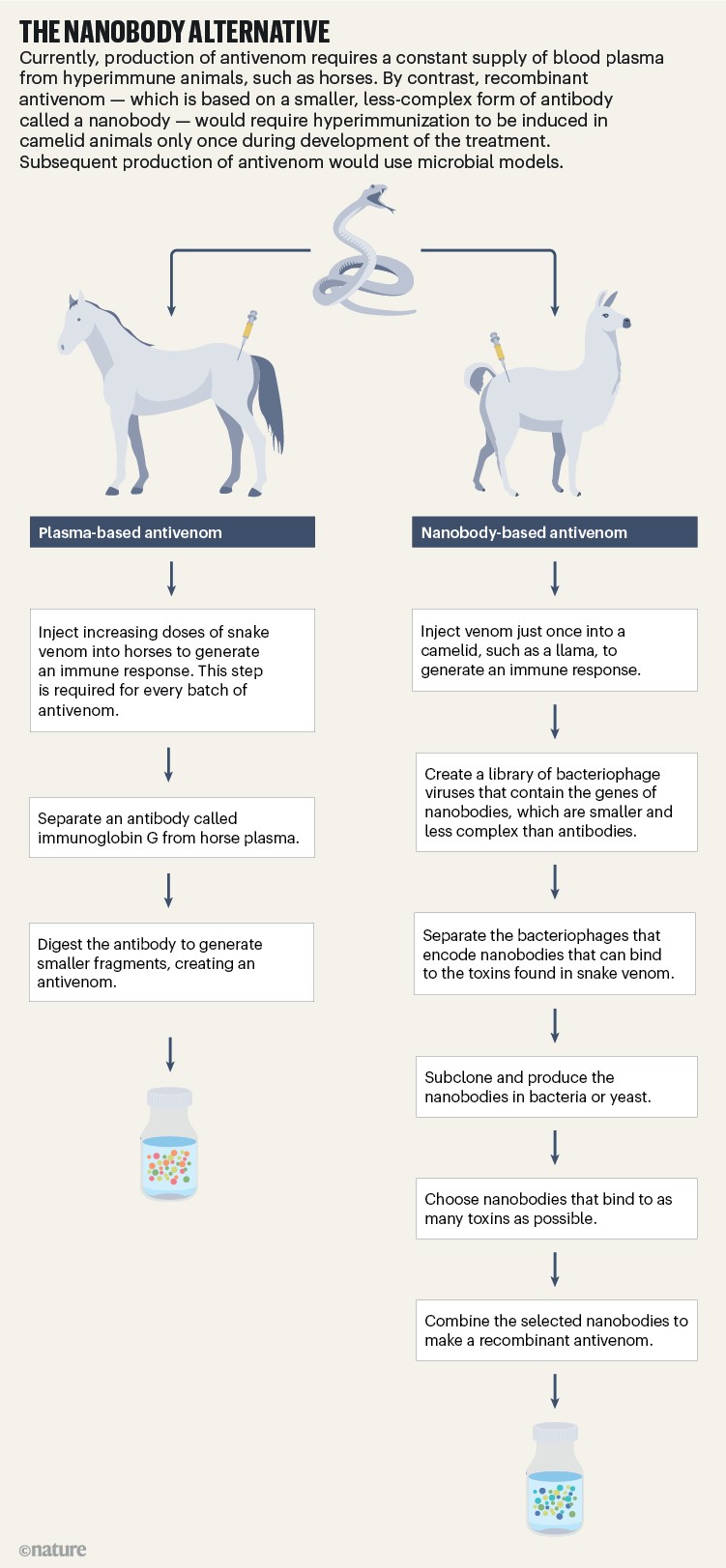
Credit score: Alisdair Macdonald
To establish nanobodies that may bind to essential toxins, Laustsen-Kiel and his colleagues first injected small quantities of venom from 18 mamba and cobra species into alpacas and llamas. Then they harvested the antibody-creating white cells from the animals’ blood. Subsequent, they took the genes from these cells and expressed them in bacteriophages — viruses that infect micro organism. “You could have a hyperlink between the protein and its DNA,” he says. “So primarily, the phage with the DNA turns into a barcode.”
As soon as this nanobody library was in place, the group started trying to find nanobodies that might bind to essentially the most medically essential toxins within the venom of African snakes. That work has but to ship outcomes, however the researchers have found nanobodies which might be able to neutralizing two of the toxin households produced by coral snakes (Micruroides sp. and Micrurus sp.), that are discovered within the Americas and are distantly associated to mambas and cobras. The 2 nanobodies mixed provided good safety in opposition to venoms from two species of coral snake8.
“Individuals previously, they thought that you’d want a whole lot of antibodies as a result of you may have technically a whole lot of medically related toxins,” Laustsen-Kiel says. “However should you’re sensible in your design, you possibly can really neutralize these venoms with fairly easy mixtures which might be possible to fabricate.”
Different teams are designing toxin blockers from scratch, with out the necessity for horses, people or alpacas. In a preprint posted in Might9, researchers led by biochemist David Baker on the College of Washington in Seattle, who additionally gained a share of the Nobel Prize in Chemistry this yr, used deep-learning fashions to create ‘mini-protein binders’. These tiny proteins act like antibodies and may bind to three-finger toxins. When the researchers produced two of those proteins and examined them in mice, they discovered that they provided good safety in opposition to the toxins. After they gave mice these mini-proteins quarter-hour after they obtained the toxins, all of the mice survived9.
Even after half-hour, each mini-proteins confirmed good safety. “That doesn’t imply that they’re going to translate right into a remedy,” Casewell says. “However I feel what’s attention-grabbing is the potential velocity with which new molecules may very well be found utilizing this strategy.” Researchers can design proteins that bind tightly to particular toxins with out having to display screen antibody or nanobody libraries.
The strategy gives different theoretical benefits, too. As a result of these proteins are smaller than antibodies, they may be capable of penetrate deeper into tissues. They’d even be cheap to provide.
Ralph, who sees the devastating impression of snakebites every day in India, is worked up that researchers are making progress in direction of new therapies. However he additionally sees a large hole between these therapies and the present normal of care. And generally it’s troublesome to see how that hole may be bridged. Snakebite is a illness related to poverty. The health-care methods in most of the international locations most affected are struggling, Ralph says. He recommends that “the main target needs to be on strengthening what at present exists”. Therapies which might be more practical or extra handy will solely be helpful if they’re additionally reasonably priced and accessible to the individuals who want them most. It’s a conundrum frequent to all uncared for tropical illnesses, and one with no apparent answer.



